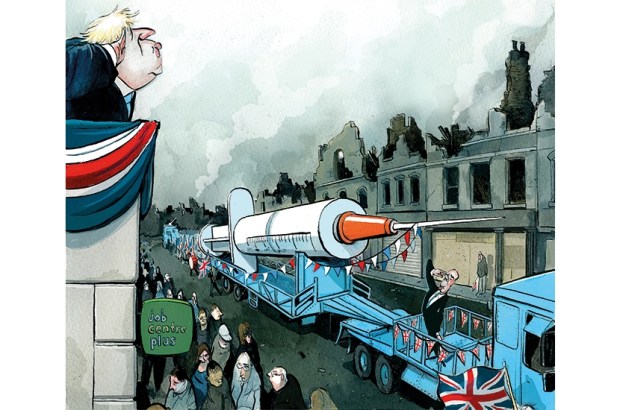
We have a vaccine. In fact, we have three — and more are on the way. While we still need to scrutinise the full data from the Pfizer, Moderna and AstraZeneca trials, the initial reports are stunning: vaccines that in some cases exceed 90 per cent effectiveness, and might be ready within weeks.
Previous surveys showed a big appetite for the vaccine, but more recent ones are concerning. According to YouGov, only 67 per cent of British people say they’d be ‘likely’ to get the Pfizer virus, with 21 per cent saying they’d be ‘fairly’ or ‘very’ unlikely to. Other polls also find that scepticism towards the vaccine is increasing.
By my amateurish, back-of-a-cigarette-packet calculations, 67 per cent is just about what we’d need for herd immunity. And that’s assuming relatively even transmission of the virus, which isn’t realistic given the clustered nature of the infections. So it would be rather helpful if we could get that 67 per cent figure quite a lot higher. How do we do it?
The first option might simply be to force people to get vaccinated. Compulsory vaccination might sound terrifyingly authoritarian, but many other democracies do it as a matter of course. In France, immunisations against measles, diphtheria, tetanus, and polio, among others, are mandatory. Since March Germany, too, has had mandatory measles vaccination — and despite the attempts of the populist Five Star Movement to abolish it, Italy’s measles vaccination law remains. Nevertheless, in the UK this doesn’t seem to be on the cards. Boris Johnson has stated that ‘there will be no compulsory vaccine’ because it’s ‘not the way we do things in this country’.
Second, there are less coercive incentives. Australia has ‘no jab, no pay’ laws, whereby parents who don’t get their kids vaccinated are no longer eligible for child and tax benefits. Brazil does something similar. The evidence indicates that the laws are effective in raising the vaccine rates. There are also some possible incentives from private firms — for instance, the CEO of Qantas is considering requiring proof of vaccination before passengers can take international flights on his planes.
But that’s about cutting people’s access to money or other rewards if they don’t get the jab. What about actively paying them to get it? There are some thorny ethical issues here: are people making a free choice when money is involved, especially if they’re poor? To what extent does a 100 per cent free choice matter anyway? Even so, the findings do point towards such policies working to boost vaccination rates — though many more high-quality studies are needed before we know the details. Such a policy might work even better if the financial reward was larger than in the published studies (£200 has been suggested). And if you’re worried about the cost, consider the alternative, which is longer lockdowns, with all their associated economic damage.
Forcing or paying people to get a vaccine does risk a backlash, however. ‘Why can’t they let us decide for ourselves?’ some might ask — while the more conspiracy-minded might imagine that if the government needs to strong-arm us into taking the vaccine, they might have something to hide about its safety. Might there be ‘softer’ ways to improve uptake, to persuade people that vaccination is worthwhile and even to convince those flirting with anti-vaccine beliefs to abandon them in favour of scientific reality?
Enter behavioural science (aka psychology). We’ve been told many times during the pandemic that behavioural insights should be at the heart of our public health response, and that for a Covid vaccine to succeed, we must look to behavioural research. OK then: let’s look at that research.
Alas, it turns out to be a rather mixed bag. The authors of a 2018 review of the studies on increasing vaccination rate noted their ‘surprise’ that so few trials had shown any success in changing how people think and feel about vaccines. These included things like educational programmes to raise awareness of the risk of disease and to demonstrate the safety of vaccines.
The authors of that review were more optimistic about the effects of some more practical interventions — ‘nudges’ — that include setting up systems with reminders to get vaccinated, having doctors explicitly recommend getting the vaccine, having people set specific dates and times for their jab, and making it easy for them to get to the clinic.
The problem is that these interventions mainly work for people who are already favourably disposed towards vaccines. What about those who aren’t convinced? Here, the research has generally failed us: despite decades of attempts, there’s not much we can say with certainty about how to persuade doubters.
Hanging over all this research is the problem of generalisability. Even if we did have rock-solid evidence of how to increase uptake of, say, the MMR vaccine in normal times, could we be sure that the same interventions would work for Covid-19? We don’t know — though we could easily argue that the prospects this time are better than usual. Getting vaccinated in 2021 won’t be like a routine health appointment; it’ll feel like your entire world is opening up again.
And that’s why I think that ultimately we won’t need to go so far as to compel UK citizens to take the vaccine to achieve herd immunity. There’ll be an unprecedented clamour to be immunised, and we can consider topping this off with cash incentives (potentially targeted at low-risk groups, like youngsters, who might not otherwise think the vaccine worthwhile).
We have a final arrow in our quiver. The Covid vaccines appear to be not only super-effective, but also super-safe. We thus find ourselves in the fortunate situation of not having to develop strategies to convince people to take a vaccine that might produce rare, devastating side effects. The worst seen in the trials were short-term fatigue, headache and muscle pain in single-digit percentages of people. The drug companies have so far been admirably transparent about these effects. Long may it continue.
We have a vaccine, it works, and it’s remarkably safe. We should thank our lucky T-cells, because it didn’t have to be this way. Although we should remain open to any strategy that can hold back this disease, the best arguments against the government forcing the vaccine on the population turn out to be the qualities of the vaccine itself.
Got something to add? Join the discussion and comment below.
Get 10 issues for just $10
Subscribe to The Spectator Australia today for the next 10 magazine issues, plus full online access, for just $10.
You might disagree with half of it, but you’ll enjoy reading all of it. Try your first month for free, then just $2 a week for the remainder of your first year.












Comments
Don't miss out
Join the conversation with other Spectator Australia readers. Subscribe to leave a comment.
SUBSCRIBEAlready a subscriber? Log in