New Zealand epidemiologist Michael Baker has just called for the government to reintroduce widespread mask mandates as Covid cases rise in an interview with Newshub journalist Rebecca Wright.
But, where is the evidence that mass indoor community masking works?
As has been the case throughout the Covid-era, only a narrow range of talking heads are given a platform in the media. Yet the truth is, the evidence on masking is tenuous at best, and most data suggests that prevention of disease is based on vulnerable and unwell populations wearing masks to protect themselves.
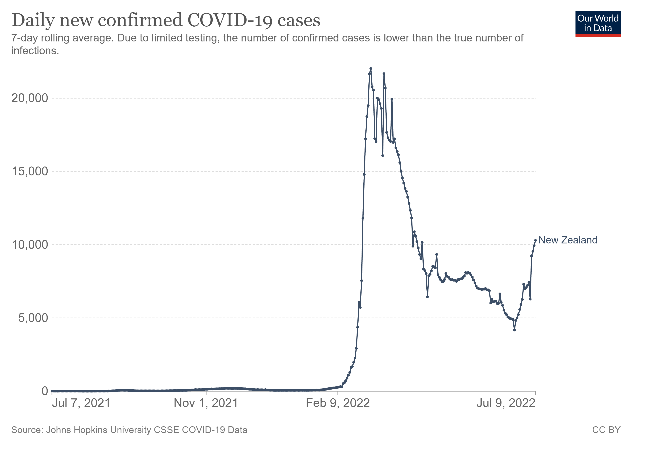
In New Zealand, the mask mandates imposed earlier this year when our students returned to education after school holidays, did not appear to work particularly well when assessing available data. As the graph shows, there was an incredible surge in infection rates from February 2022.
I recently lodged an Official Information Act request with the Minister for the Covid-19 Response to understand the extent of published and peer-reviewed scientific evidence on masking efficacy that underpinned the decision to introduce the mandate.
I wanted to understand what data and analyses had been provided to the Minister in the course of the pandemic that demonstrated community-based masking prevented hospitalisation and death.
What knowledge did the Minister have about the efficacy of mask-wearing for people who have previously had Covid?
I was also interested in the potential for harm from mask-wearing in educational settings, including for mental health and for groups with hearing loss, and whether masking slowed learning and development.
The Minister responded, saying:
‘Neither I nor my Cabinet colleagues undertake scientific research or studies. Therefore, your request is refused under section 18(g) of the Act, on the grounds that the information requested is not held by my office.’
A list of domestic and international studies (largely from 2020), were attached.
Instead of tangible, physical data, the Minister added:
‘I am advised that as part of reviewing international evidence, the Ministry considers other advice from international organisations including the Centres for Disease Control and Prevention, Public Health England, the European Centre of Disease Control and Prevention, Australian jurisdictions, and a range of scientific and medical journals. The information is collated through Ministry specialist technical advisory groups whose membership includes a variety of expert professions such as infection prevention and control, public health, vaccine and immunology, testing and diagnostics, infectious diseases, microbiology, therapeutics, and clinical care, and primary care. Independent literature searches and ongoing reviews of the science are also undertaken regularly. When reviewing evidence, the Ministry ensures it is applicable to the New Zealand situation and can be applied in our context.’
This is startling. The Minister for the Covid-19 Response, along with the wider Covid-19 Health Response Act, had extraordinary powers during the pandemic to issue orders that the public were required to follow, such as community mask wearing. The degree to which that Minister is informed – or ignorant – impacts the quality of these powers.
Where is the specific (rather than general) analysis discussing the success or lack thereof, of the earlier back-to-school strategy that required widespread masking?
Ministers must be able to show that there is solid evidence for policy and law. Mandates, which require students and workers to wear masks all day and on public transport impose a toll on civil society: they are not only uncomfortable, but they slow and alter the free flow of communication between human beings.
It is one thing popping out to the shop and putting your mask on for 10 minutes. Forcing a healthy person to wear a mask all day is morally and ethically questionable.
Michael Baker might advocate for mask-wearing, but it is the Minister for Covid-19 Response who must agree. Accountability promotes trust in civil society. What are the implications of these government interventions?
I’ve previously written that it is well understood Covid does not pose a risk to most people, particularly those who are young and healthy with school-aged children (and younger) being the least at-risk. Forcing otherwise healthy people to wear face masks that they repeatedly touch and refit in between touching multiple surfaces, especially when their mask becomes humid from constant wear, seems patently unfair and unhygienic.
One of the quoted studies from the Norwegian Institute of Public Health stated:
‘Randomised trials from community settings indicate a small protective effect. There is no reliable evidence of the effectiveness of non-medical facemasks in community settings. There is likely to be substantial variation in effectiveness between products.’
And:
‘Potential undesirable effects of facemasks include the risks of incorrect use, a false sense of security (leading to relaxation of other interventions), and contamination of masks. In addition, some people experience problems breathing, discomfort, and problems with communication.’
Baker reverts to the ‘two basics’: If you’re sick don’t go out, and we have to turn into a mask-using society.
Firstly, Baker ignores the early viral replication stage which means we are most infectious when we have no idea; and secondly, he assumes that everyone lives a comfortable existence where they will be financially and otherwise supported.
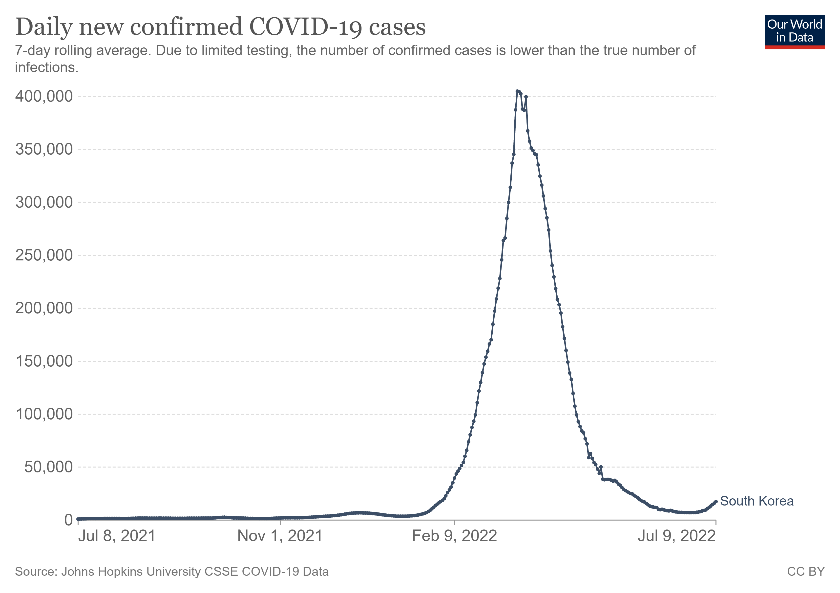
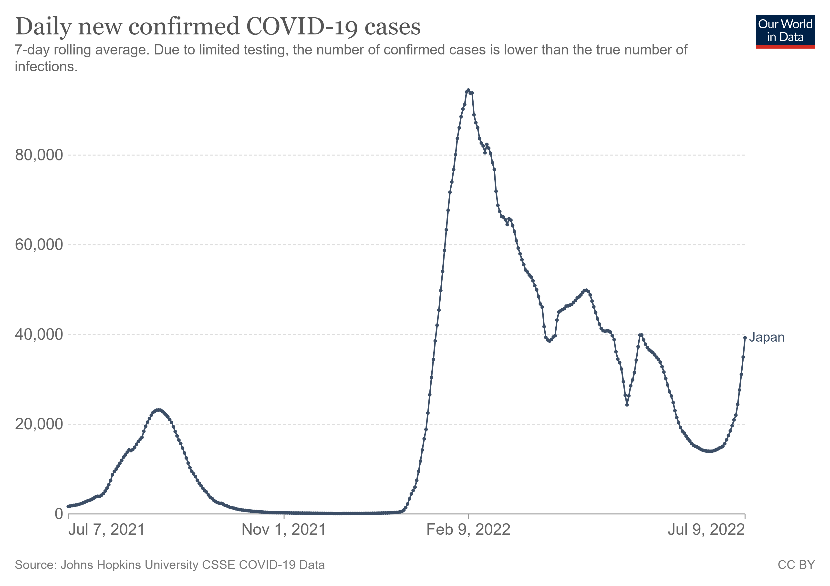
Importantly, claiming absolute success for mask-wearing in Japan and South Korea is a topic of open debate. I’m not sure the evidence stacks up. Our World in Data graphs demonstrate that Sars-Cov-2 infection waves occurred despite persistent mask mandates.
Why didn’t the Newshub journalist challenge Baker’s claims?
What we can observe is a pattern of peak Omicron, despite mask wearing. Masks cannot stop a Covid wave – and have failed to do so statistically across the world – but the media return again and again to the mask issue and sidestep important conversations about early treatment to arrest Sars-Cov-2 in the early viral phase.
There is no question that there is tremendous stress on the hospital system, on staff, and patients. But this is not only from Covid.
Baker’s claim that ‘one in a thousand people who contract Sars-Cov-2 are dying from it could be seen as hyperbolic, given the enormity of asymptomatic infections that are presumed missing from the data.
‘If you go out when you have this infection and you infect your friends and family and other people, you are going to be killing some people,’ ought to have been challenged by the journalist.
Treatments with a long history of safe use that keep people out of hospital have been available since January 2021, but ‘personal responsibility’ is fairly difficult when early treatment [1] is kept out of the picture.
Covid is a complex disease, and people become sick to different degrees – that’s why doctors need the discretion to treat the multifactorial viral, inflammatory and thrombotic conditions (among others) that present in front of them. But New Zealand’s medical institutions have weakened the autonomy of medical doctors during this pandemic.
The Ministry of Health has not advocated or supplied vitamin D to workers, to low-income and immunodeficient groups, despite its well-known ability to prevent lower respiratory tract infections – where major harm occurs for both Covid and influenza.
It’s time the government backed away from mandate dogma and started acknowledging that Covid is different for everyone and that crackdowns on doctors are likely to be the greater driver of hospitalisations and death.
Jodie Bruning is a New Zealand based sociologist and is a trustee of Physicians & Scientists for Global Responsibility (PSGR.org.nz). Papers and writing can be found at Brownstone Institute, TalkingRisk.NZ and at JRBruning.Substack.com and at Talking Risk on Rumble.
[1] References for early treatments.
McCullough, P.A. et al. (2020) Multifaceted highly targeted sequential multidrug treatment.
Association of American Physicians and Surgeons. Physician List & Guide to Home-Based COVID Treatment.
Canadian Covid Care Alliance. Early Treatment Protocols.
World Council for Health. Early Covid-19 treatment guidelines: A practical approach to home-based care for healthy families.
Front Line COVID-19 Critical Care Alliance. Prevention & Treatment Protocols for COVID-19.
Alexander P.E. et al. (2021). Early ambulatory outpatient sequenced antiviral multidrug COVID-19 treatment (including for Delta or similar variants) for high-risk children and adolescents
Got something to add? Join the discussion and comment below.
Get 10 issues for just $10
Subscribe to The Spectator Australia today for the next 10 magazine issues, plus full online access, for just $10.

























Comments
Don't miss out
Join the conversation with other Spectator Australia readers. Subscribe to leave a comment.
SUBSCRIBEAlready a subscriber? Log in