Listen
Like many of my fellow junior doctors, I trusted a Conservative government with the NHS. If it’s to stay strong and up to date, a health service cannot remain static. It needs not just money but carefully thought-out reform — as well as a strong economy to support it.
Just after the general election, David Cameron laid out the problem as he saw it: a ‘weekend effect’ where a patient admitted to hospital on a Sunday is 16 per cent more likely to die than one admitted on a Wednesday. ‘So seven-day care isn’t just about a better service — it’s about saving lives,’ he said. This is a classic example of a little knowledge being a dangerous thing.
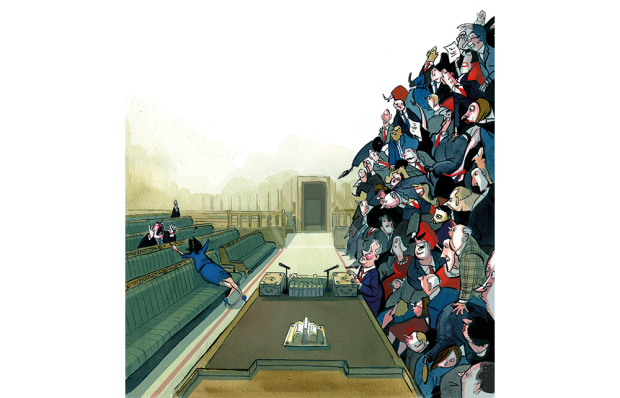
When I work weekend shifts, I do notice that services could be improved — not everyone in a hospital works seven days. But if Jeremy Hunt wants to remedy this, he should incentivise more doctors to work out of hours. Instead, he plans to penalise those of us who already do. Yes, pay for normal hours will rise by 11 per cent — but ‘normal hours’ will be defined as lasting until 10 p.m., Monday to Saturday. This will, of course, mean less money for doctors who work late into evenings. But even more importantly, it will deter junior doctors from pursuing specialisms with more out-of-hours work — such as accident and emergency, paediatrics, and acute medicine.
Junior doctors training in A&E already work the most evenings, nights and weekends. Currently they are rewarded financially for this, in the same way that most workers — from cleaners to policemen — are. But without the out-of-hours premium, a career in A&E becomes even less appealing. The NHS is already facing a recruitment and retention crisis. Dr Cliff Mann, Britain’s most senior casualty medic, recently explained that half of all our trainee A&E doctors abandon the profession after four years. It’s tough, harrowing work — and making it pay less will not address the recruitment crisis. He calculates that some 600 consultants and trainee A&E doctors have emigrated in five years.
Fewer trainees in A&E means more gaps in the staff rota, which will have to filled with expensive locum doctors — resulting in a higher cost to the taxpayer. A cap on locum rates (something Jeremy Hunt has introduced from next April) will just make these gaps harder to fill. Market forces govern locum rates. It seems strange that the Tories would try to cap prices when they can usually grasp free-market economics: price-fixing leads to shortages.
It costs about £230,000 to train a doctor — and that investment will be lost if British doctors keep fleeing abroad. At the last count, almost a quarter of specialist doctors in Australia came from the UK. If things go on like this, the budget for training doctors might be recategorised as overseas aid.
As I quickly found out, being a junior doctor often means working long past your allotted hours. You stay until the job is done, whether or not you’re paid for the overtime. We stay because we care. If we strike, then, as we may well do, it won’t be because we’re greedy but because we can’t bear to see the service we love damaged so badly.
Got something to add? Join the discussion and comment below.
Get 10 issues for just $10
Subscribe to The Spectator Australia today for the next 10 magazine issues, plus full online access, for just $10.
Katia Florman is a junior doctor at a London teaching hospital.
You might disagree with half of it, but you’ll enjoy reading all of it. Try your first month for free, then just $2 a week for the remainder of your first year.












Comments
Don't miss out
Join the conversation with other Spectator Australia readers. Subscribe to leave a comment.
SUBSCRIBEAlready a subscriber? Log in