My great-grandfather did not fight in the war. He wasn’t a conscientious objector — he was a scientist helping to develop radar. It’s tempting to imagine family history repeating itself. I’m not alongside my colleagues on the NHS front line; instead I’ve been part of a large team at the Crick Institute, helping to develop tests for Sars-CoV-2, the causative agent of Covid-19. For the first phase of our struggle against this virus, we’ve had minimal testing capacity — no radar — and we’ve suffered the consequences.
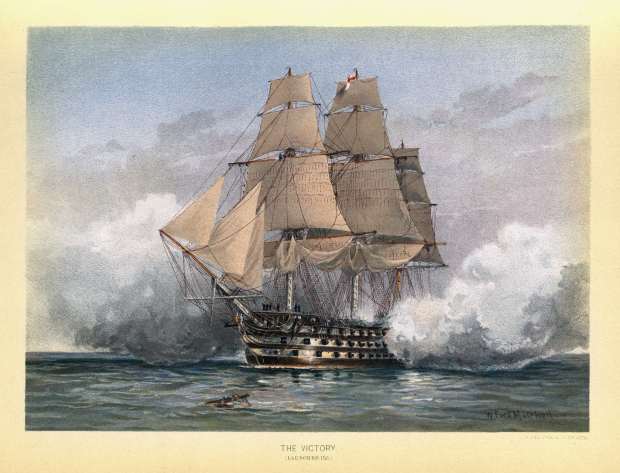
The director of our institute, Sir Paul Nurse, borrowed another wartime analogy when he imagined academic labs as a flotilla of ‘little ships’, as at Dunkirk, that could be set up quickly to help rescue a rather desperate situation. The protocols we’ve developed have been downloaded more than 5,000 times, and we’ve helped other testing laboratories (including the big ones that are now coming online) with re-agents and scientific advice. We’ve been able to get recovering doctors and nurses back to work quicker, and crucially we’ve been able to identify healthcare workers who may have been spreading the virus unwittingly to the most vulnerable.
The team at the Crick is extremely multi-national. Wartime analogies are not helpful when they promote national exceptionalism, still less when they imply an individual battle between patient and virus. They are helpful when it comes to getting people to think clearly and act swiftly. The frustration when we’ve run up against what might be politely described as ‘NHS bureaucracy’ has been intense. When we’ve dealt with local NHS partners who are determined and dynamic, we’ve been able to save lives. In this sense there really is a war on, and for once I’m happy to see politicians treat it in this way.
We will win this war through immunity. Understanding immunity to respiratory viruses is really difficult — more like decoding Enigma than developing radar. We will need new technology as well as optimising existing tests. So far, the best tests can give a reasonable estimate of whether someone has been exposed to the virus. They cannot yet tell you if you are immune to it. The trouble with coronaviruses is that they have evolved to evade immunity. They possess all sorts of unknown weaponry that dampens down our immune responses.
Humanity has never developed ‘herd immunity’ to any coronavirus, and each of the four ‘seasonal’ coronaviruses that we’ve all had in childhood (and subsequently) can re-infect us throughout our lifetime. This was experimentally demonstrated for the seasonal coronavirus strain called 229E, which usually causes a mild infection — just like Sars-CoV-2 does in the majority of cases. Volunteers were infected with 229E, and duly developed symptoms. They also developed antibodies a couple of weeks later. They were then able to be re-infected a few months later (albeit they developed milder symptoms). So far there are no confirmed cases of reinfection with Sars-CoV-2, but the virus has been with us a very short time (yes, I know it feels like an age). My prediction would be that for patients who have only mild, or indeed no, symptoms of Covid-19, they will probably not develop a strong and lasting enough immune response to prevent reinfection in several months’ time.
It’s possible to have a ‘positive’ antibody test without having been infected by Sars-CoV-2. Scientists at my institute have demonstrated that antibodies generated against the four seasonal coronaviruses can to an extent cross-react. This might have important consequences for immunity, but it certainly makes simple antibody tests more difficult to interpret. Scientists are trying to make the tests as specific as possible, but it’s not a trivial problem to solve. Roche and Abbott, two commercial giants in the field, have introduced antibody tests that offer a significant improvement. It’s worth noting that both of these tests target an internal protein of the virus, whereas antibodies for the main entry weapon of the virus — appropriately called Spike — aren’t directly tested. It’s antibodies to Spike that are expected to protect you. That means we really cannot assume that they measure immunity, even if they might be a good indicator of whether you had the virus.
The best correlation of immunity that we know about so far isn’t a simple antibody test. You culture the virus in a high containment facility, and use minute amounts of serum extracted from blood to see if it will prevent the virus from replicating. Even this ‘neutralisation assay’ isn’t perfect, but it tells you if the antibodies you’ve raised in your blood block the virus — usually a pretty good indication of immunity. It’s very low throughput, so in the lab we are working on making it slightly higher throughput: still not good enough for testing patients at scale, but useful for research purposes. Other laboratories are working on neutralisation of what are called viral ‘pseudo particles’. The theory is that these look enough like the virus itself that neutralising them is a good predictor of immunity.
We need a vaccine. Immunity through infection probably isn’t good enough, even if you were prepared to countenance the many hundreds of thousands of deaths that allowing the virus to spread though the UK would entail. The really good news about this virus is that it’s not mutating in such a way as to make vaccination especially difficult. There are at least 90 vaccine candidates, and some are likely to be successful. A simple vaccine made from killed virus has already demonstrated some protection in animal models in China, and more sophisticated vaccines such as those being developed in Oxford and Imperial are also very promising. A massive effort to increase production capacity in advance is being put in place across the globe.
But how long will it take? A colleague in San Diego offered me a wager. I think we will have an effective vaccine rolled out within 18 months; he thinks it will be closer to four years. The stake, a case of (in)appropriately branded beer, isn’t very important when you consider what else depends on the answer. I’m confident: if we are very lucky, there may even be a reasonably effective vaccine available for a significant number of vulnerable people by September.
Optimism isn’t a strategy though. We have to be realistic: a cure isn’t just around the corner. Antiviral drugs such as Remdesivir are not going to be transformative. They might help a bit, especially if they can be given early, but the data so far is that at best they will give a marginal benefit.
What about face masks? There is strong evidence for medical masks, but they are in short supply. It’s probable that if enough people wear homemade cloth masks this will reduce transmission by a small but useful amount. Still not a viable strategy by itself. But we can’t remain in permanent lockdown — it’s not just the economy that will suffer, there are serious health consequences too. South Korea and other countries that have implemented a really effective test, track and trace policy have fought the virus to a standstill. Their economies will be able to reopen cautiously. Ours will remain shut until we can emulate their success; a naive attempt to reopen would almost immediately result in a dreaded second peak. So what do we do?
Even worse than optimism would be cynicism, fatalism and despair. We will soon have enough testing capacity. Deploying it effectively will be the next challenge. It will be crucial to focus the increased testing capacity on people who have a high chance of transmitting the virus to vulnerable people — that means healthcare workers, especially those with low symptoms or even no symptoms of the virus. More accurate antibody tests could be combined with a really determined approach to testing for the virus in the general population. Unlike the cynics, I think that the NHS app being trialled on the Isle of Wight could help a lot. I shall certainly download it, and I would encourage everyone to do the same. No doubt it won’t be perfect, but alternative approaches will be much worse.
The success of the lockdown doesn’t just come with an economic cost: it also costs lives. We have been severely hampered in our ability to deliver elective care, including cancer screening and therapy, transplant services and surgery. The NHS has not been overwhelmed, but in truth it’s been a close-run thing. It is a dangerous fantasy to think that either the economy or the NHS could do well if we allowed the virus to spread exponentially — tantamount to surrendering to a ruthless enemy.
Until we have a vaccine, we must find ways to reopen our economy and our NHS without letting the virus spread uncontrollably. That’s going to require a meticulous, data-driven approach. One avoidable blunder in the early stages of our response was not to acquire enough data: we didn’t have sufficient testing capacity. I applaud the recent efforts to rectify this mistake. We are going to need technology-driven testing, tracking and tracing, with social distancing where we can, and wearing masks where we can’t. It’s a good strategy — let’s pursue it with hope.
Got something to add? Join the discussion and comment below.
Get 10 issues for just $10
Subscribe to The Spectator Australia today for the next 10 magazine issues, plus full online access, for just $10.
SPECTATOR.CO.UK/podcast
Rupert Beale and former cabinet minister Nicky Morgan on immunity and the way out.
You might disagree with half of it, but you’ll enjoy reading all of it. Try your first month for free, then just $2 a week for the remainder of your first year.





Comments
Don't miss out
Join the conversation with other Spectator Australia readers. Subscribe to leave a comment.
SUBSCRIBEAlready a subscriber? Log in